
Innovative Advancements for Value-based Healthcare
Health, Health Policy Transformation, Innovation at LMI
Value-based programs are opening new pathways to high-quality healthcare.
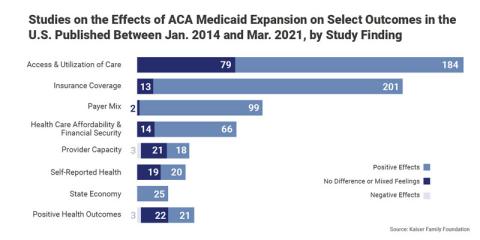
Over the past several years, the U.S. government transformed the country’s health system through the Affordable Care Act—a paradigm shift enabling value-based care and purchasing programs to improve patient outcomes, support healthier populations, and create new avenues for cost savings.
Value-based care, or pay-for-performance care, encourages improving individual and population health outcomes by linking payments for services with quality for patients and rewarding providers for improved care delivery, which can lower costs. Value-based purchasing, the other component of this shift, works similarly by linking payments for provider purchases to improvements in quality-of-care metrics.
These components enable the Centers for Medicare & Medicaid Services (CMS) to implement payment reforms based on value. Value-based purchasing also incentivizes providers to promote preventive care, including regular testing and screenings to catch health concerns earlier. Treating issues proactively is easier and less expensive, leading to lower lifetime healthcare costs and better patient outcomes (rather than reacting when a health concern becomes urgent and costly to treat).
Center Care Quality on the Patient
Madeline Leonard, a health policy consultant at LMI, says that one of the biggest lessons many providers have learned over the past few years is the importance of prioritizing patients and focusing on care quality. While centering any healthcare response on patients may seem obvious, pressure from multiple healthcare crises can pivot systems away from care quality to deal with immediate issues instead.
"The important thing to understand about improving healthcare quality is that patients of all types have to be at the center of the conversation. From there, providers and program administrators can work on finding innovative ways to improve participation and bring costs down," Leonard says.
During the pandemic, telehealth emerged as a critical lifeline, connecting patients and providers across the country. Leonard says that making telehealth services permanent and widely available could enable patients to access routine care at a lower total cost. Underserved patients are often disadvantaged given a lack of nearby providers and the cost required to get to offices, including time off work and the monetary cost of travel and care for dependents. Telehealth helps bridge those gaps. Providers, too, can expand the ways they work with patients, thus improving the quality of care and patient outcome metrics important for value-based care.
Stay Flexible
In November, the United States Department of Health and Human Services finalized payment rules to expand access to behavioral healthcare, cancer screening coverage, and dental care. The expansion treats the whole patient and gives both patients and providers more flexibility in care available and Medicare and Medicaid coverage.
As part of the 2022 CMS Behavioral Health Strategy, CMS is strengthening access to vital behavioral health services. By allowing behavioral health clinicians, like licensed professional counselors and marriage and family therapists, to offer services under the general (rather than direct) supervision of the Medicare practitioner, CMS makes it easier for Medicare beneficiaries to obtain these services. Further, to increase participation in rural and underserved areas, CMS is finalizing an adjustment to providers' quality score if they participate in the shared savings program.
According to Leonard, expanding how providers participate in programs and align with value-based care goals can improve access to care. "We have learned from the implementation of the shared savings program that there are many ways for providers and program administrators to work together to improve patient access and outcomes," she says.
Bundle Services to Cut Costs and Improve Patient Outcomes
Heather Ensley, a senior consultant in the healthcare advisory group at LMI, adds that bundling services can also reduce costs. She notes that, as value-based care has become more widely adopted, value-based purchasing frameworks have incentivized providers to bundle interrelated healthcare services together, increasing the ease of receiving care and lowering the total cost.
"There are ways we can expand this to purchasing as well and realize similar outcomes," Ensley says. "Recent rulemaking is meant to incentivize providers to be able to tell patients the total cost of care within a given range. Value-based purchasing plays a role because providers have to estimate what they need to provide quality care."
Improving healthcare outcomes through value-based care requires ongoing integration between providers and Medicare and Medicaid. The initial work in this area has expanded coverage and enhanced flexibility. By keeping patients and care quality at the center of the conversation, providers can bundle services based on individual patient needs and find innovative ways to reduce costs.
LMI has more than two decades of experience analyzing diverse healthcare data to inform health program and policy improvements. We work at the intersection of science, policy, logistics, and analytics to facilitate innovation in healthcare provision and payment, implement federal healthcare priorities, advance health security, and optimize service delivery and program effectiveness.

Zaki Saleh
Sr. Vice President, Health & Civilian MarketZaki Saleh leads LMI’s health & civilian market, where he is responsible for profit and loss management and business growth, overseeing project delivery, execution, and overall customer satisfaction as well as the business development function.


